National Vital
Statistics Reports
Volume 71, Number 4 August 4, 2022
Fetal Mortality: United States, 2020
by Elizabeth C.W. Gregory, M.P.H., Claudia P. Valenzuela, M.P.H., and Donna L. Hoyert, Ph.D.,
Division of Vital Statistics
Abstract
Objectives—This report presents 2020 fetal mortality data
by maternal race and Hispanic origin, age, tobacco use during
pregnancy, and state of residence, as well as by plurality, sex,
gestational age, birthweight, and selected causes of death.
Trends in fetal mortality are also examined.
Methods—Descriptive tabulations of data are presented
and interpreted for all fetal deaths reported for the United States
for 2020 with a stated or presumed period of gestation of 20
weeks or more. Cause-of-fetal-death data only are restricted to
residents of the 43 states and the District of Columbia, where
cause of death was based on the 2003 fetal death report revision
and less than 50% of deaths were attributed to Fetal death of
unspecified cause (P95).
Results—A total of 20,854 fetal deaths at 20 weeks of
gestation or more were reported in the United States in 2020. The
2020 U.S. fetal mortality rate was 5.74 fetal deaths at 20 weeks
of gestation or more per 1,000 live births and fetal deaths, which
was not significantly different from the rate of 5.70 in 2019. The
fetal mortality rate in 2020 for deaths occurring at 20–27 weeks
of gestation was 2.97, essentially unchanged from 2019 (2.98).
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
National Vital Statistics System
NCHS reports can be downloaded from: https://www.cdc.gov/nchs/products/index.htm.
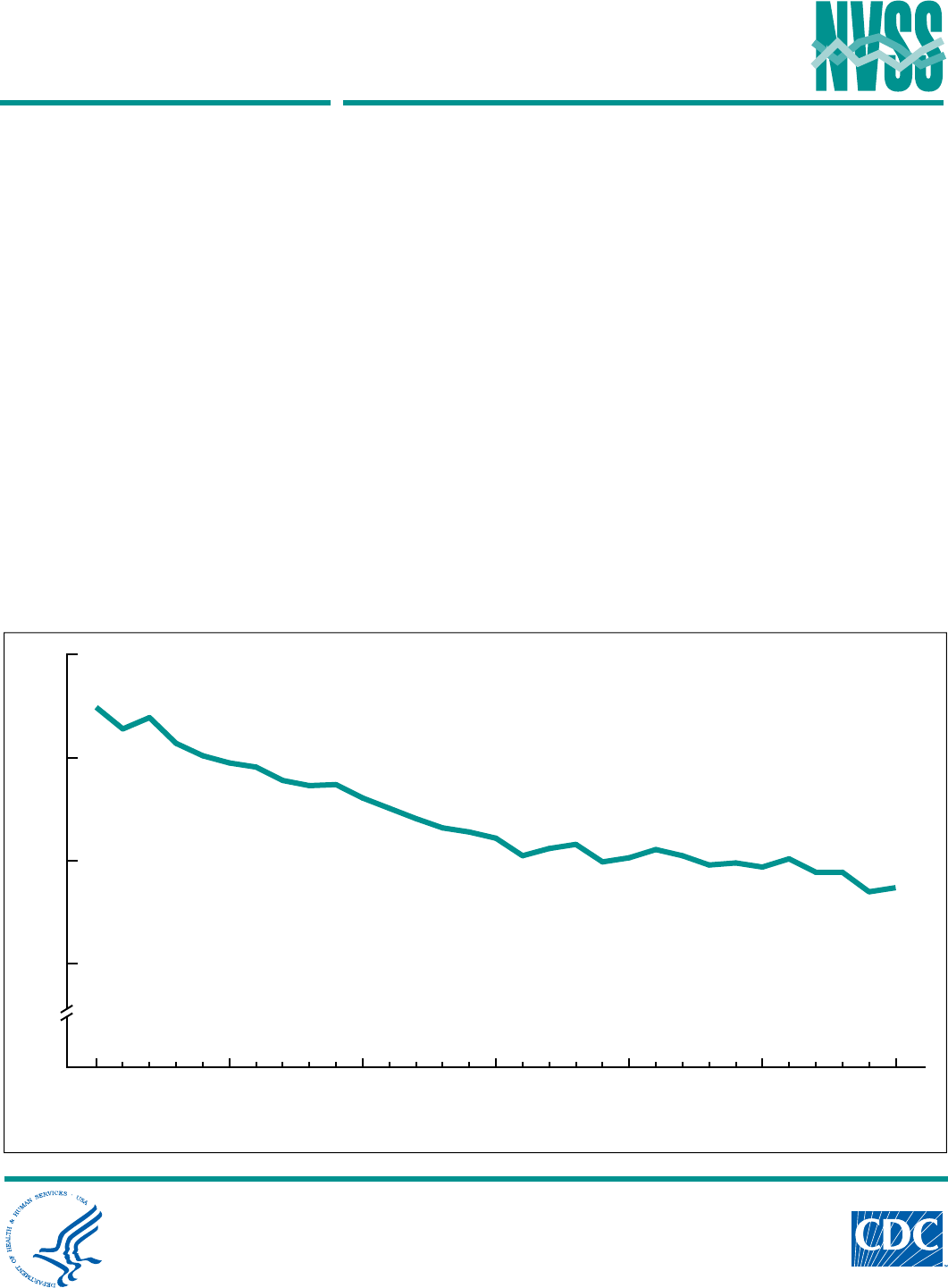
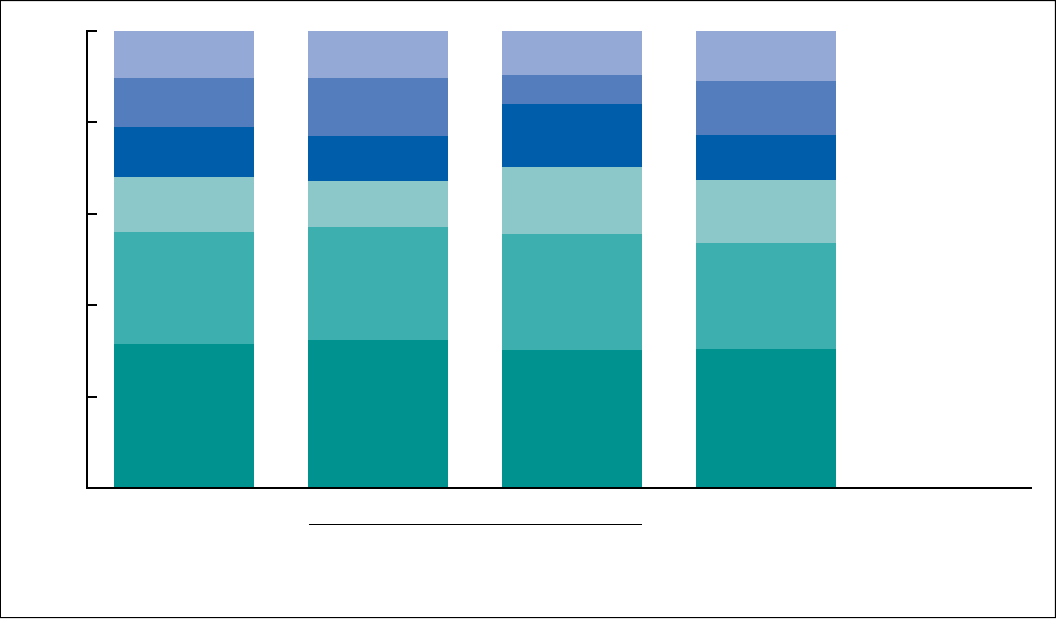
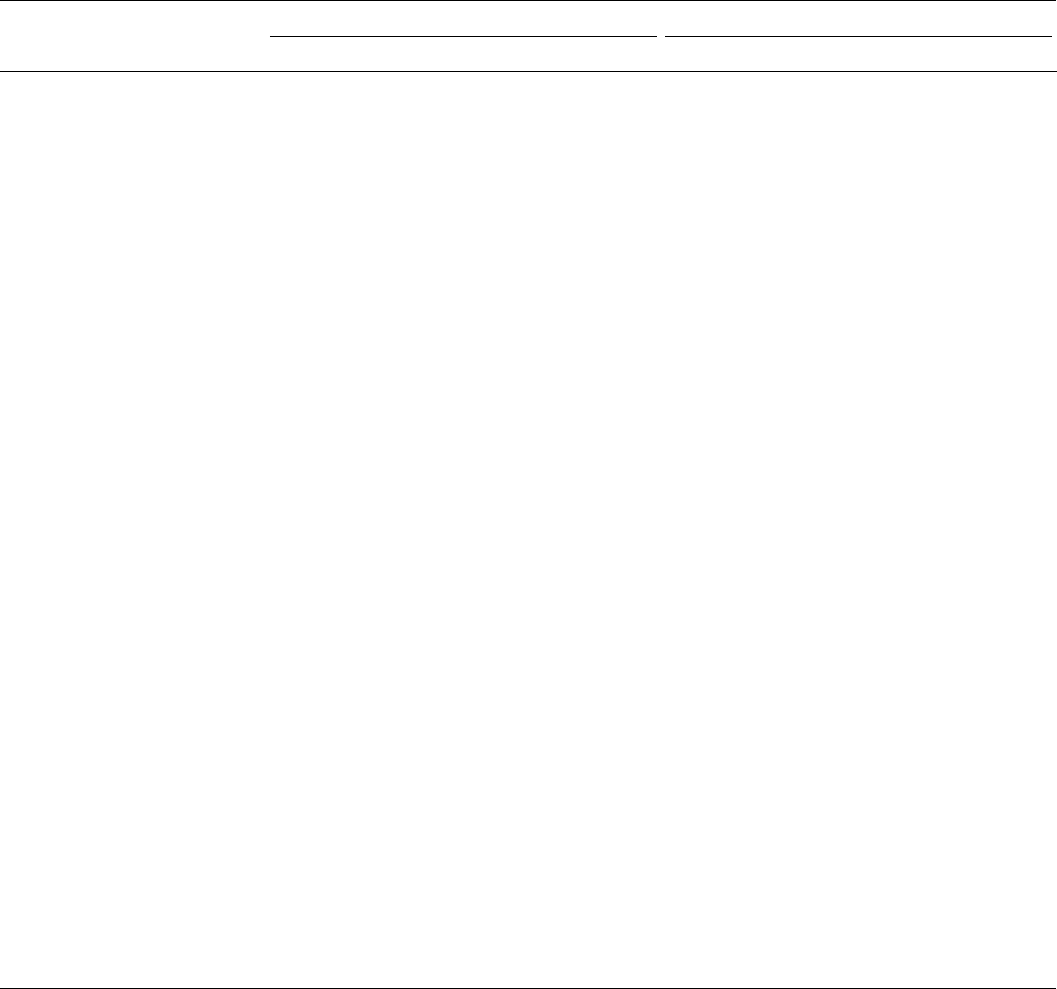
Figure 1. Fetal mortality rate: United States, 1990–2020
0
5
6
7
8
2020201520102005200019951990
Rate per 1,000 live births and fetal deaths
NOTE: Fetal mortality rate is the number of fetal deaths at 20 weeks of gestation or more per 1,000 live births and fetal deaths.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
2 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
For deaths occurring at 28 weeks of gestation or more, the rate in
2020 (2.78) was not significantly different from 2019 (2.73). In
2020, the fetal mortality rate was highest for non-Hispanic Native
Hawaiian or Other Pacific Islander (10.59) and non-Hispanic
Black (10.34) women and lowest for non-Hispanic Asian
women (3.93). Fetal mortality rates were highest for females
under 15 and aged 45 and over, for women who smoked during
pregnancy, and for women with multiple gestation pregnancies.
Five selected causes accounted for 89.6% of fetal deaths in the
43-state and District of Columbia reporting area.
Keywords: fetal death • stillbirth • pregnancy loss • National
Vital Statistics System
Introduction
Fetal mortality—the intrauterine death of a fetus at any
gestational age—is a major but often overlooked public health
issue. Much of the public concern surrounding reproductive loss
has focused on infant mortality, due in part to lesser knowledge
of the incidence, etiology, and prevention strategies for fetal
mortality. This report presents detailed data on numbers and
rates of fetal deaths for the United States for 2020. Data are
presented by maternal race and Hispanic origin, age, tobacco use
during pregnancy, and state of residence, as well as by plurality,
sex, gestational age at delivery, birthweight, and selected causes
of death. Trends in fetal mortality are also examined.
In addition to the tabulations included in this report, more
detailed analysis of fetal mortality is possible by using the annual
fetal death public-use file. The data file may be downloaded from:
https://www.cdc.gov/nchs/data_access/Vitalstatsonline.htm.
The public-use file does not include geographic detail; a file with
this information may be available upon special request (see the
Division of Vital Statistics data release policy: https://www.cdc.
gov/nchs/nvss/dvs_data_release.htm). Fetal death data may also
be accessed via the Centers for Disease Control and Prevention’s
(CDC) Wide-ranging Online Data for Epidemiologic Research
(WONDER). WONDER is a web-based data query system that
makes CDC data available to public health professionals and the
public (1).
Methods
Data sources
Data in this report are drawn from two National Center
for Health Statistics (NCHS) vital statistics data files: the 2020
fetal death data set (for fetal deaths) and the 2020 birth data set
(for births). The 2020 fetal death data set contains information
from all reports of fetal death filed in the 50 states, the District
of Columbia, Guam, and Puerto Rico (American Samoa did not
report data for 2020, and data for the Northern Marianas and
U.S. Virgin Islands were excluded to protect confidentiality due
to the small number of events reported) (2). The 2020 birth data
set contains information from all Certificates of Live Birth filed
in the 50 states, the District of Columbia, Guam, the Northern
Marianas, Puerto Rico, and the Virgin Islands (American Samoa
did not report data for 2020). Tables showing data by jurisdiction
also provide separate information for Guam and Puerto Rico;
however, these data are not included in U.S. totals.
Fetal mortality
Fetal death refers to the intrauterine death of a fetus
prior to delivery (Technical Notes). Fetal mortality is generally
divided into three periods based on gestational age: less than
20 completed weeks of gestation, 20–27 weeks of gestation
(early fetal deaths), and 28 weeks of gestation or more (late fetal
deaths). Although the vast majority of fetal deaths occur early
in pregnancy, most states in the United States only require the
reporting of fetal deaths at 20 weeks of gestation or more (2),
and fetal mortality data from the National Vital Statistics System
are usually presented for fetal deaths at 20 weeks of gestation
or more. Therefore, only fetal deaths reported at 20 weeks of
gestation or more are included in this report. Numbers and rates
for early and late fetal deaths are shown separately for selected
variables. Statistics on fetal death exclude data for induced
terminations of pregnancy. Fetal mortality rates in this report are
computed as the number of fetal deaths at 20 weeks of gestation
or more per 1,000 live births and fetal deaths at 20 weeks or
more (Technical Notes).
Data limitations
Variation exists among states in reporting requirements
and possibly in completeness of reporting of fetal death data,
and these variations can have implications for data quality and
completeness (Technical Notes). Correct interpretation of fetal
death data should include an evaluation of the completeness
of reporting of fetal deaths, as well as an evaluation of the
completeness of reporting for the specific variables of interest
(3–5). The percentage of not-stated responses for fetal death
data varies markedly among variables and states; see “User
Guide to the 2020 Fetal Death Public Use File”(2).
2003 revision of U.S. Standard Report of Fetal
Death
Starting in 2018, all 50 states, the District of Columbia,
Guam, the Northern Marianas, Puerto Rico, and the Virgin
Islands reported data based on the 2003 U.S. Standard Report
of Fetal Death.
With the implementation of the 2003 revision, two
worksheets, the Patient’s Worksheet (6) and the Facility
Worksheet (7), were developed to encourage collection of data
from the best sources. For the Patient’s Worksheet, data are
directly obtained from the mother and include items such as
mother’s date of birth, race, Hispanic origin, level of education,
tobacco use during pregnancy, and place of residence. For the
Facility Worksheet, data are obtained from the medical records
of the mother for items such as prenatal care, medical risk
factors, maternal morbidity, plurality, sex of fetus, gestational
age, birthweight, and cause of death. Detailed definitions for data
items that are collected from the Facility Worksheet are in the
“Guide to the Facility Worksheet” (8).
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 3
This report uses the latest fetal death data to present
information on fetal deaths and fetal death rates by race and
Hispanic origin, maternal age, tobacco use during pregnancy,
plurality, sex of fetus, gestational age, birthweight, state of
residence, and selected causes of death.
Race and Hispanic origin
The 2003 revision of the U.S. Standard Report of Fetal Death
allows the reporting of more than one race (multiple races) for the
mother (9) in accordance with the revised standards issued by the
Office of Management and Budget (OMB) in 1997 (10). Starting
in 2018, all 50 states and the District of Columbia, Guam, the
Northern Marianas, Puerto Rico, and the Virgin Islands reported
race data in accordance with these 1997 OMB standards, which
require the reporting of a minimum of five race categories and
allow for reporting of race by either single race (reported alone)
or in combination (more than one race or multiple races) (10).
The race and Hispanic-origin groups shown in this report follow
the 1997 standards and differ from the bridged-race categories
shown in previous reports (11). The new categories are
non-Hispanic single-race White, non-Hispanic single-race
Black or African American, non-Hispanic single-race American
Indian or Alaska Native (AIAN), non-Hispanic single-race Asian,
non-Hispanic single-race Native Hawaiian or Other Pacific
Islander (NHOPI), and Hispanic (for brevity in text, references to
the race groups omit “single race”).
Race and Hispanic origin are reported independently on the
report of fetal death. Most tables in this report show data for
the categories of non-Hispanic White, non-Hispanic Black, and
Hispanic. Selected tables also include data for the categories
non-Hispanic AIAN, non-Hispanic Asian, and non-Hispanic
NHOPI. Data are also presented in some tables for Hispanic
subgroups: Mexican, Puerto Rican, Cuban, Central and South
American, Dominican, and Other and unknown Hispanic. Data
were presented separately for Dominican women for the first
time beginning with the 2018 data year. Data for this subgroup
had previously been included in the category Other and unknown
Hispanic.
Fetal deaths by state
Comparisons of fetal mortality rates by state can be affected
by differences in reporting requirements for fetal deaths among
registration areas, particularly for fetal deaths occurring at
gestational ages early in the reporting period (Technical Notes).
Additionally, the small numbers of fetal deaths in some states
by year can result in lack of reliability for state-specific fetal
mortality rates. To try to address these issues, in addition to
showing fetal mortality rates at 20 weeks or more by state for
2020, this report also presents fetal deaths and fetal mortality
rates by state for fetal deaths at 24 weeks of gestation or more
for the latest combined 3-year period (2018–2020).
Cause of death
NCHS codes the cause of fetal death reported by the certifier
using the International Classification of Diseases, 10th Revision
(ICD–10) (12). In this report, the 5 most frequently reported
causes of death shown, including unspecified cause, are drawn
from 45 causes in the List of 124 Selected Causes of Fetal
Death as defined in Instruction manual, part 9 (13) and ranked
according to the number of fetal deaths.
Data on the five causes of death are included for the 43
states and the District of Columbia that reported cause of death
based on the 2003 revision of the U.S. Standard Report of Fetal
Death and met the reporting requirement of having less than 50%
of records assigned to unspecified cause (P95). This reporting
area includes 15,740 fetal deaths, representing 75.5% of all fetal
deaths in 2020. These statistics based on a subnational area
are not generalizable to the entire United States. In tables and
figures, the five selected causes are shown in descending order
according to the number of deaths assigned to each cause.
Statistical significance
Statements in this report have been tested for statistical
significance. A statement that a given mortality rate is higher or
lower than another rate indicates that the rates are significantly
different unless otherwise noted. For information on the methods
used to test for statistical significance, as well as more detailed
information on the collection, interpretation, and availability of
fetal death data, see the 2020 User Guide (2).
Results
Trends in fetal mortality
• In 2020, 20,854 fetal deaths occurring at 20 weeks of
gestation or more were reported in the United States, a
decline of 3% from 2019 (21,478) (Table 1, Figure 1).
• The fetal mortality rate was 5.74 fetal deaths at 20 weeks of
gestation or more per 1,000 live births and fetal deaths in
2020, which was not significantly different from the 2019
rate of 5.70. With minor fluctuations, the total U.S. fetal
mortality rate has declined 23% since 1990 (7.49).
• The early fetal mortality rate (20–27 weeks of gestation)
was essentially unchanged from 2019 (2.98) to 2020 (2.97).
This rate declined 6% from 2014 (3.16) to 2020.
• The late fetal mortality rate (28 weeks of gestation or more)
was 2.78 in 2020, which was not significantly different from
the 2019 rate of 2.73. The late fetal mortality rate has been
essentially unchanged since 2014 (2.83).
Race and Hispanic origin
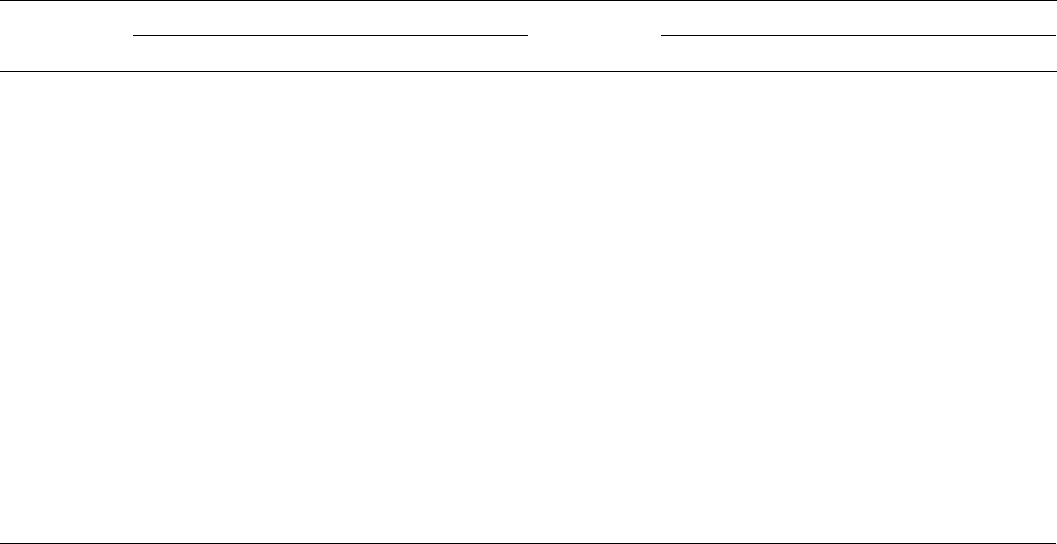
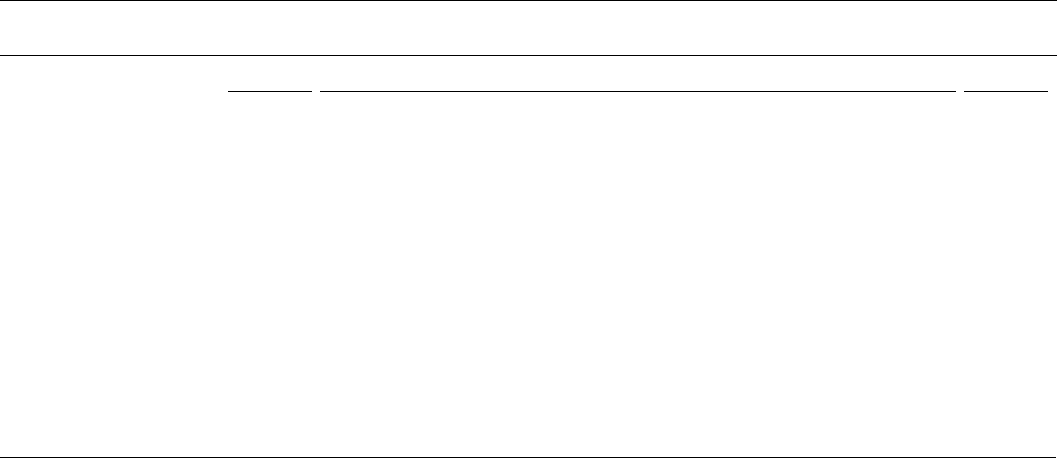
• From 2019 to 2020, no significant changes in fetal mortality
rates were observed for non-Hispanic White (4.71 to
4.73), non-Hispanic Black (10.41 to 10.34), non-Hispanic
AIAN (7.47 to 7.84), non-Hispanic Asian (4.02 to 3.93),
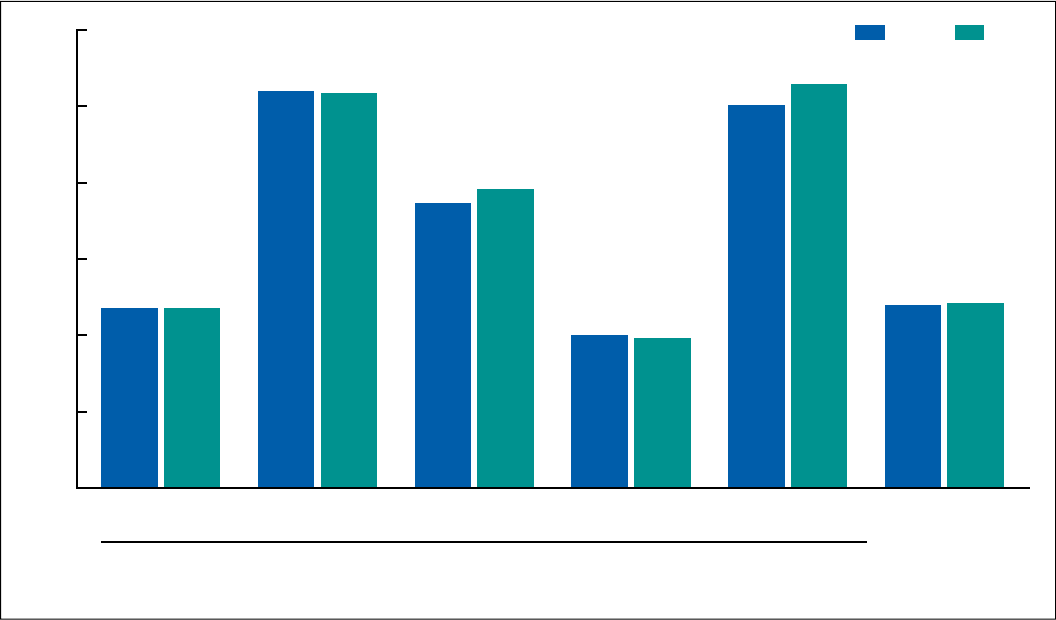
4 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
non-Hispanic NHOPI (10.03 to 10.59), and Hispanic (4.79 to
4.86) women (Table 2, Figure 2).
• Among Hispanic-origin subgroups from 2019 to 2020, no
significant changes in fetal mortality rates were seen for
Mexican (4.86 to 4.79), Puerto Rican (5.17 to 4.98), Cuban
(4.71 to 5.23), Dominican (4.75 to 4.41), Central and South
American (4.12 to 4.49), and Other and unknown Hispanic
(5.29 to 5.87) women (Table 3).
• In 2020, fetal mortality rates continued to vary by race and
Hispanic origin; rates were highest for non-Hispanic NHOPI
(10.59) and non-Hispanic Black (10.34) women, followed
by non-Hispanic AIAN (7.84) women.
• The rate was lowest for non-Hispanic Asian women (3.93),
followed by non-Hispanic White (4.73) and Hispanic (4.86)
women.
• Among Hispanic-origin subgroups in 2020, rates ranged
from 4.41 for Dominican women to 5.87 for Other and
unknown Hispanic women; however, differences among the
groups were generally not significant.
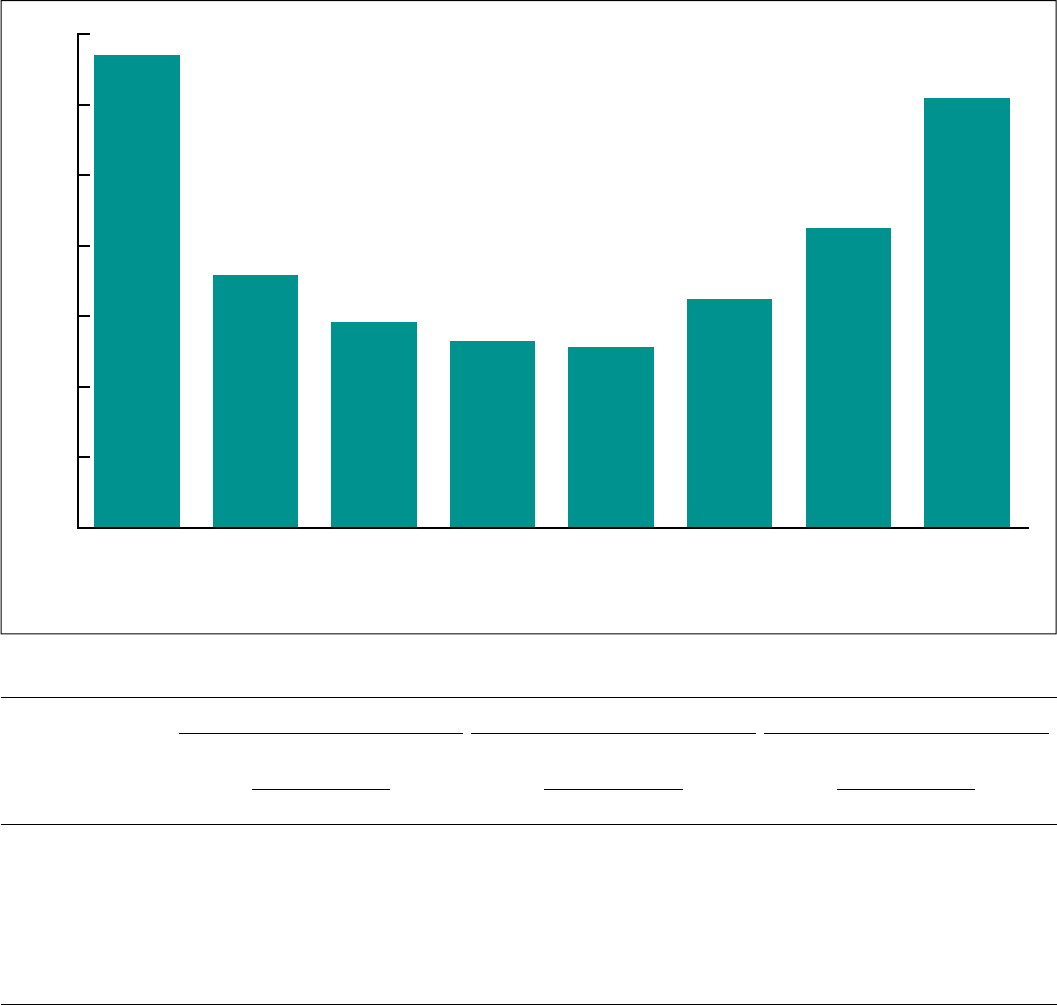
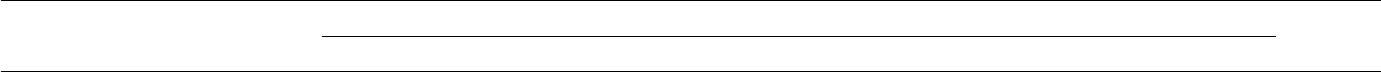
Maternal age
• In 2020, fetal mortality rates varied by maternal age. Rates
were highest for females under age 15 (13.42) and aged
45 and over (12.20) and lowest for women aged 25–29
(5.29) and 30–34 (5.12) (Table 4, Figure 3).
• The fetal mortality rate for teenagers aged 15–17 (7.61) was
44%–49% higher and the rate for teenagers aged 18–19
(7.02) was 33%–37% higher than the rates for women aged
25–29 (5.29) and 30–34 (5.12).
• Age-specific rates for non-Hispanic Black women were
higher than those for non-Hispanic White women for those
aged 15 and over. Rates for non-Hispanic Black women
were higher than those for Hispanic women for those aged
15–44; rates for women aged 45 and over in both groups
were not significantly different. The number of events
was too small (fewer than 20 events in the numerator) to
calculate reliable rates for females under age 15 for all three
race and Hispanic-origin groups.
Tobacco use during pregnancy
• The fetal mortality rate for women who smoked during
pregnancy (8.71) was more than one and one-half times
higher than that for women who did not smoke during
pregnancy (5.10) (Table 5).
• The pattern was similar for the three largest race and
Hispanic-origin groups. The fetal mortality rate for women
who smoked during pregnancy compared with those who
did not was more than one and one-half times higher for
non-Hispanic White women (7.65 and 4.12, respectively)
and non-Hispanic Black women (14.68 and 9.40), and more
than twice as high for Hispanic women (9.50 and 4.50).
See Table 5 for fetal mortality rates by tobacco use during
pregnancy by age.
Figure 2. Fetal mortality rates, by race and Hispanic origin of mother: United States, 2019 and 2020
0
2
4
6
8
10
12
SOURCE: National Center for Health Statistics, National Vital Statistics System.
White Black Asian
HispanicNative Hawaiian or
Other Pacific Islander
American Indian
or Alaska Native
Non-Hispanic
Rate per 1,000 live births and fetal deaths in specified group
4.71
4.73
10.41
10.34
7.47
7.84
4.02
3.93
10.03
10.59
4.79
4.86
2019
2020
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 5
Plurality
• The fetal mortality rate for twins (12.12) was more than
twice that for singletons (5.51) (Table A). The rate for triplet
or higher-order deliveries (28.72) was more than five times
that for singletons.
• The pattern was similar for the three largest race and
Hispanic-origin groups. For example, the fetal mortality rate
for twins compared with singletons was more than twice as
high for non-Hispanic White (10.02 and 4.53, respectively)
and Hispanic (12.73 and 4.65) women, and more than one
and one-half times as high for non-Hispanic Black (16.34
and 10.06) women.
Table A. Fetal mortality rates, by selected characteristics and race and Hispanic origin of mother: United States, 2020
Fetal mortality rates
1
Fetal deaths Live births
Non-Hispanic,
single race
2
Non-Hispanic,
single race
2
Non-Hispanic,
single race
2
Characteristic All races
3
White Black Hispanic
4
All races
3
White Black Hispanic
4
All races
3
White Black Hispanic
4
Plurality . . . . . . . . . . . . . . . 5.74 4.73 10.34 4.86 20,854 8,753 5,536 4,231 3,613,647 1,843,432 529,811 866,713
Single . . . . . . . . . . . . . . . 5.51 4.53 10.06 4.65 19,389 8,101 5,158 3,947 3,498,335 1,781,686 507,736 845,516
Twin . . . . . . . . . . . . . . . . 12.12 10.02 16.34 12.73 1,380 608 358 267 112,437 60,082 21,554 20,709
Triplet or higher . . . . . . . 28.72 25.76 36.97 * 85 44 20 17 2,875 1,664 521 488
Sex of fetus . . . . . . . . . . . . 5.74 4.73 10.34 4.86 20,854 8,753 5,536 4,231 3,613,647 1,843,432 529,811 866,713
Male . . . . . . . . . . . . . . . . 5.88 4.83 10.79 4.94 10,936 4,589 2,939 2,190 1,848,092 945,464 269,341 441,401
Female . . . . . . . . . . . . . . 5.59 4.62 9.87 4.78 9,918 4,164 2,597 2,041 1,765,555 897,968 260,470 425,312
Male–female ratio . . . . . 1.05 1.05 1.09 1.03 … … … … … … … …
* Estimate does not meet National Center for Health Statistics standards of reliability or precision; based on fewer than 20 fetal deaths in the numerator.
… Category not applicable.
1
Rate per 1,000 live births and fetal deaths in specified group.
2
Race and Hispanic origin are reported separately on the report of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race
categories are consistent with the 1997 Office of Management and Budget standards; see Technical Notes in this report. Single race is defined as only one race reported on the report of fetal
death.
3
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
4
Includes all people of Hispanic origin of any race; see Technical Notes in this report.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
Figure 3. Fetal mortality rates, by age of mother: United States, 2020
Rate per 1,000 live births and fetal deaths in specified group
SOURCE: National Center for Health Statistics, National Vital Statistics System.
Age group
0
2
4
6
8
10
12
14
45 and over40–4435–3930–3425–2920–2415–19Under 15
13.42
7.16
5.83
5.29
5.12
6.48
8.49
12.20
6 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
Sex of fetus
• In 2020, the fetal mortality rate for male fetuses was
5.88, which was 5% higher than for female fetuses (5.59)
(Table A).
• The fetal mortality rate for male fetuses compared with
female fetuses was 5% higher for non-Hispanic White (4.83
and 4.62, respectively) and 9% higher for non-Hispanic
Black (10.79 and 9.87) women. No significant difference
was seen for Hispanic women (4.94 and 4.78).
Period of gestation
• In 2020, just over one-half (51.6%) of all fetal deaths at 20
weeks of gestation or more occurred at 20–27 weeks (early
fetal deaths) and 48.4% occurred at 28 weeks of gestation
or more (late fetal deaths) (Table 6).
• The fetal mortality rate was highest at 20–23 weeks of
gestation (540.18), declined to a low at 39–40 (0.60) and
41 weeks of gestation (0.66), and then increased to 4.38 at
42 weeks of gestation or more.
Birthweight
• In 2020, more than one-third (35.6%) of fetal deaths at 20
weeks of gestation or more weighed less than 500 grams
(1 lb. 1 oz.) at delivery, and nearly one-half (47.0%) weighed
less than 750 grams (1 lb. 12 oz.) (Table 6).
• The fetal mortality rate was highest for fetuses weighing less
than 500 grams (590.00) and decreased with increasing
birthweight to a low of 0.58 for fetuses weighing 3,500–3,999
grams. Fetal mortality rates then increased slightly for fetuses
weighing 4,000 grams or more (1.30).
Fetal mortality rates by state
• For combined years 2018–2020, the U.S. fetal mortality rate
for fetal deaths at 24 weeks or more was 3.67 fetal deaths
at 24 weeks of gestation or more per 1,000 live births and
fetal deaths (Table B).
• For combined years 2018–2020, fetal mortality rates were
highest (above 5.00) in the District of Columbia (5.05),
Arkansas (5.23), Alabama (5.37), and Mississippi (6.57),
Area Fetal deaths Fetal mortality rate
1
New Jersey . . . . . . . . . . . 1,118 3.73
New Mexico . . . . . . . . . . 168 2.47
New York . . . . . . . . . . . . 2,439 3.70
North Carolina . . . . . . . . 1,499 4.21
North Dakota . . . . . . . . . 123 3.93
Ohio . . . . . . . . . . . . . . . . 1,644 4.11
Oklahoma . . . . . . . . . . . . 587 3.99
Oregon . . . . . . . . . . . . . . 405 3.26
Pennsylvania . . . . . . . . . 1,481 3.68
Rhode Island . . . . . . . . . 110 3.56
South Carolina . . . . . . . . 754 4.43
South Dakota . . . . . . . . . 118 3.43
Tennessee . . . . . . . . . . . . 1,036 4.30
Texas . . . . . . . . . . . . . . . 3,157 2.80
Utah . . . . . . . . . . . . . . . . 515 3.67
Vermont . . . . . . . . . . . . . 50 3.13
Virginia . . . . . . . . . . . . . . 956 3.26
Washington . . . . . . . . . . 817 3.21
West Virginia . . . . . . . . . 199 3.69
Wisconsin . . . . . . . . . . . . 660 3.50
Wyoming . . . . . . . . . . . . 67 3.47
American Samoa . . . . . . --- ---
Guam . . . . . . . . . . . . . . . 105 11.36
Northern Marianas . . . . . --- ---
Puerto Rico . . . . . . . . . . 344 5.63
Virgin Islands . . . . . . . . . --- ---
Area Fetal deaths Fetal mortality rate
1
Total . . . . . . . . . . . . . . . . . . 41,041 3.67
Alabama . . . . . . . . . . . . . 939 5.37
Alaska . . . . . . . . . . . . . . . 109 3.70
Arizona . . . . . . . . . . . . . . 955 4.01
Arkansas . . . . . . . . . . . . . 572 5.23
California . . . . . . . . . . . . 4,282 3.23
Colorado . . . . . . . . . . . . . 597 3.18
Connecticut . . . . . . . . . . 271 2.64
Delaware . . . . . . . . . . . . . 140 4.41
District of Columbia . . . . 138 5.05
Florida . . . . . . . . . . . . . . 2,734 4.18
Georgia . . . . . . . . . . . . . . 1,777 4.72
Hawaii . . . . . . . . . . . . . . . 185 3.72
Idaho . . . . . . . . . . . . . . . 224 3.43
Illinois . . . . . . . . . . . . . . . 1,447 3.45
Indiana . . . . . . . . . . . . . . 912 3.77
Iowa . . . . . . . . . . . . . . . . 333 2.98
Kansas . . . . . . . . . . . . . . 369 3.47
Kentucky . . . . . . . . . . . . . 614 3.86
Louisiana . . . . . . . . . . . . 615 3.48
Maine . . . . . . . . . . . . . . . 120 3.36
Maryland . . . . . . . . . . . . 857 4.07
Massachusetts . . . . . . . . 604 2.94
Michigan . . . . . . . . . . . . . 1,218 3.77
Minnesota . . . . . . . . . . . . 673 3.41
Mississippi . . . . . . . . . . . 722 6.57
Missouri . . . . . . . . . . . . . 836 3.88
Montana . . . . . . . . . . . . . 107 3.19
Nebraska . . . . . . . . . . . . 231 3.09
Nevada . . . . . . . . . . . . . . 448 4.27
New Hampshire . . . . . . . 111 3.11
Table B. Fetal deaths at 24 weeks of gestation or more and fetal mortality rates, by state or territory: United States, 2018–2020
--- Data not available.
1
Rate per 1,000 live births and specified fetal deaths.
NOTES: Fetal deaths with not-stated period of gestation are proportionally distributed to less than 24 weeks and 24 weeks or more; see Technical Notes in this report. Numbers may not add to
totals due to rounding.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 7
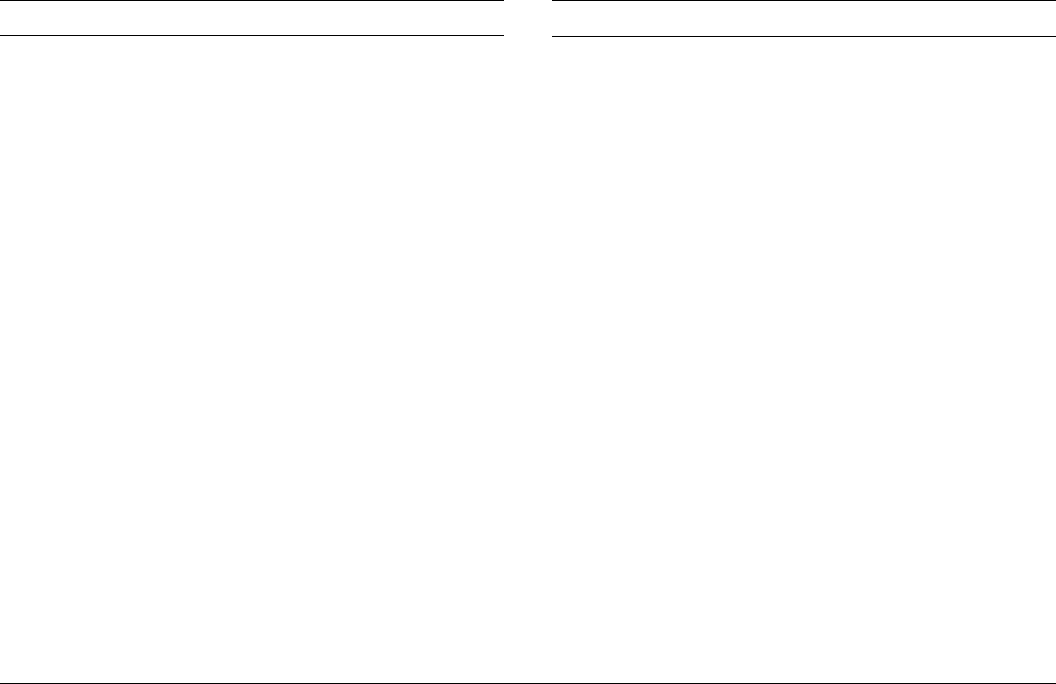
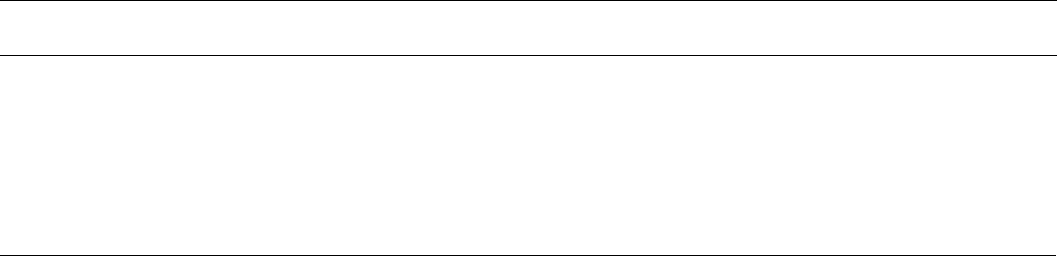
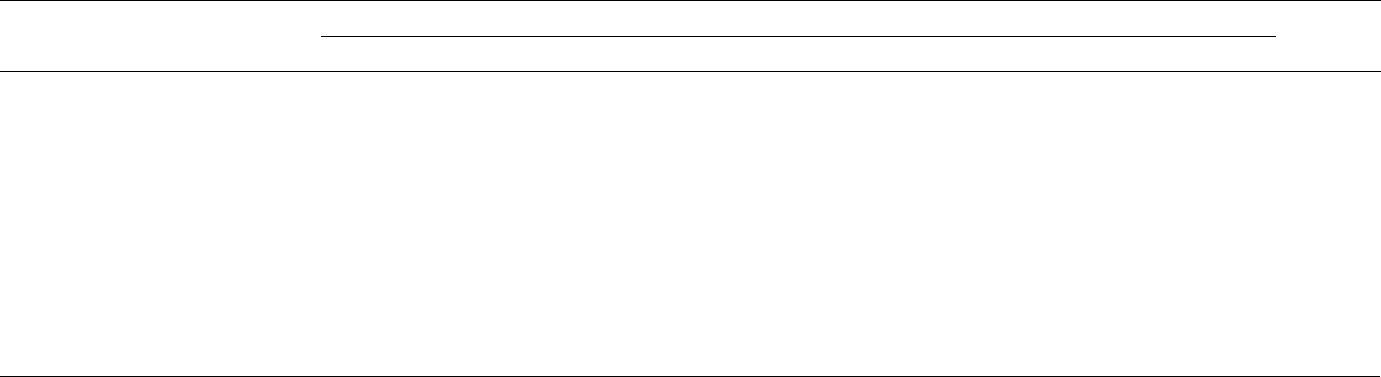
• Congenital malformations was the third most common
cause for fetal deaths to non-Hispanic White women,
followed by maternal complications and maternal
conditions unrelated to pregnancy.
• Among non-Hispanic Black women, maternal
complications was the third most common cause of
fetal death, maternal conditions unrelated to pregnancy
was fourth, and congenital malformations was fifth.
• Among Hispanic women, maternal complications was
the third most common cause of fetal death, congenital
malformations was fourth, and maternal conditions
unrelated to pregnancy was fifth.
References
1. Centers for Disease Control and Prevention. CDC
WONDER: Fetal deaths information. Available from:
https://wonder.cdc.gov/fetal.html.
2. National Center for Health Statistics. User guide
to the 2020 fetal death public use file. Hyattsville,
MD. 2022. Available from: https://ftp.cdc.gov/pub/
Health_Statistics/NCHS/Dataset_Documentation/DVS/
fetaldeath/2020fetaluserguide.pdf.
3. Makelarski JA, Romitti PA, Caspers KM, Puzhankara S,
McDowell BD, Piper KN. Use of active surveillance
methodologies to examine over-reporting of stillbirths on
fetal death certificates. Birth Defects Res A Clin Mol Teratol
91(12):1004–10. 2011.
and lowest (below 3.00) in New Mexico (2.47), Connecticut
(2.64), Texas (2.80), Massachusetts (2.94), and Iowa (2.98).
• See Table 7 for fetal deaths at 20 weeks of gestation or more
by state and territory for 2020.
Selected causes of fetal death
• The five most common selected causes of fetal death
accounted for 89.6% of fetal deaths in the 43-state and
District of Columbia reporting area (Table 8, Figure 4).
By order of frequency, these were: 1) Fetal death of
unspecified cause (unspecified cause); 2) Fetus affected
by complications of placenta, cord and membranes
(placental, cord and membrane complications); 3) Fetus
affected by maternal complications of pregnancy (maternal
complications); 4) Fetus affected by maternal conditions that
may be unrelated to present pregnancy (maternal conditions
unrelated to pregnancy); and 5) Congenital malformations,
deformations and chromosomal abnormalities (congenital
malformations).
• The five most common selected causes of fetal death and
the top two causes were the same for non-Hispanic White,
non-Hispanic Black, and Hispanic women, while the ranking
of the other causes differed (Table 8, Figure 4).
• Unspecified cause and placental, cord and membrane
complications were the two most common of the
selected causes for all three groups.
Figure 4. Percent distribution of fetal deaths, by selected causes of death and race and Hispanic origin of mother:
43 states and the District of Columbia, 2020
0
20
40
60
80
100
HispanicBlackWhite
Total
Percent
NOTE: Codes in parentheses are cause-of-death codes as classified by the International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
Non-Hispanic
All others
11.1
11.7
9.9
13.6
23.2
30.5
9.7
6.3
13.8
14.6
25.4
30.2
10.4
12.6
9.8
10.0
24.8
32.4
10.4
10.6
10.9
12.1
24.4
31.6
Maternal complications
(P01)
Placental, cord and
membrane complications
(P02)
Maternal conditions
unrelated to pregnancy
(P00)
Congenital malformations
(Q00–Q99)
Unspecified cause (P95)
8 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
4. Heuser CC, Hunn J, Varner M, Hossain S, Vered S, Silver
RM. Correlation between stillbirth vital statistics and
medical records. Obstet Gynecol 116(6):1296–301. 2010.
5. Lydon-Rochelle MT, Cárdenas V, Nelson JL, Tomashek
KM, Mueller BA, Easterling TR. Validity of maternal and
perinatal risk factors reported on fetal death certificates.
Am J Public Health 95(11):1948–51. 2005.
6. National Center for Health Statistics. Patient’s worksheet
for the report of fetal death. 2019. Available from:
https://www.cdc.gov/nchs/data/dvs/fetal-death-mother-
worksheet-english-2019-508.pdf.
7. National Center for Health Statistics. Facility worksheet
for the report of fetal death. 2019. Available from:
https://www.cdc.gov/nchs/data/dvs/fetal-death-facility-
worksheet-2019-508.pdf.
8. National Center for Health Statistics. Guide to completing
the facility worksheets for the Certificate of Live Birth
and Report of Fetal Death (2003 revision). Hyattsville,
MD: National Center for Health Statistics. 2019.
Available from: https://www.cdc.gov/nchs/data/dvs/
GuidetoCompleteFacilityWks.pdf.
9. National Center for Health Statistics. 2003 revision of the
U.S. Standard Report of Fetal Death. Available from: https://
www.cdc.gov/nchs/data/dvs/FDEATH11-03finalACC.pdf.
10. Office of Management and Budget. Revisions to the
standards for the classification of federal data on race and
ethnicity. Fed Regist 62(210):58782–90. 1997.
11. MacDorman MF, Gregory ECW. Fetal and perinatal
mortality: United States, 2013. National Vital Statistics
Reports; vol 64 no 8. Hyattsville, MD: National Center for
Health Statistics. 2015.
12. World Health Organization. International statistical
classification of diseases and related health problems,
10th revision. Geneva, Switzerland. 2009.
13. National Center for Health Statistics. Instruction manual,
part 9: ICD–10 cause-of-death lists for tabulating mortality
statistics (updated September 2020 to include WHO
updates to ICD–10 for data year 2019). Available from:
https://www.cdc.gov/nchs/data/dvs/Part9Instruction
Manual2019-508.pdf.
14. National Center for Health Statistics. Model State Vital
Statistics Act and Regulations, 1992 Revision. Public Health
Service. PHS 94–1115. Hyattsville, MD. 1994. Available
from: https://www.cdc.gov/nchs/data/misc/mvsact92b.pdf.
15. Kowaleski J. State definitions and reporting requirements
for live births, fetal deaths, and induced terminations of
pregnancy (1997 revision). Hyattsville, MD: National Center
for Health Statistics. 1997. Available from: https://www.
cdc.gov/nchs/data/misc/itop97.pdf.
16. National Center for Health Statistics. Report of the Panel to
Evaluate the U.S. Standard Certificates. 2000.
17. Hoyert DL. Perinatal mortality in the United States, 1985–
91. National Center for Health Statistics. Vital Health Stat
20(26). 1995. Available from: https://www.cdc.gov/nchs/
data/series/sr_20/sr20_026.pdf.
18. Martin JA, Osterman MJK, Kirmeyer SE, Gregory
ECW. Measuring gestational age in vital statistics data:
Transitioning to the obstetric estimate. National Vital
Statistics Reports; vol 64 no 5. Hyattsville, MD: National
Center for Health Statistics. 2015.
19. National Center for Health Statistics. Editing specifications
for fetal death records [unpublished]. Hyattsville, MD.
2020.
20. National Center for Health Statistics. User guide to the
2017 fetal death public use file. Hyattsville, MD. 2019.
Available from: https://ftp.cdc.gov/pub/Health_Statistics/
NCHS/Dataset_Documentation/DVS/fetaldeath/2017Fetal
UserGuide.pdf.
21. National Center for Health Statistics. User guide to the
2018 fetal death public use file. Hyattsville, MD. 2020.
Available from: https://ftp.cdc.gov/pub/Health_Statistics/
NCHS/Dataset_Documentation/DVS/fetaldeath/2018Fetal
UserGuide.pdf.
List of Detailed Tables
1. Number of fetal deaths and births and fetal mortality rates
for 1990–2020 and early and late fetal deaths and fetal
mortality rates for 2014–2020: United States ........... 9
2. Fetal deaths and mortality rates, by race and Hispanic origin
of mother: United States, 2018–2020 ................. 10
3. Fetal deaths and mortality rates, by Hispanic origin of
mother: United States, 2018–2020 ................... 11
4. Total, early, and late fetal deaths and mortality rates, by
age and race and Hispanic origin of mother: United States,
2020 12. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
5. Fetal mortality rates, by tobacco use during pregnancy,
age, and race and Hispanic origin of mother: United States,
2020 13. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
6. Fetal deaths and mortality rates, by birthweight, gestational
age, and race and Hispanic origin of mother: United States,
2020 14. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
7. Fetal deaths at 20 weeks of gestation or more and fetal
mortality rates: United States and each state and territory,
2020 16. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8. Fetal deaths and percentage of total deaths for the five
selected causes, by race and Hispanic origin of mother: 43
states and the District of Columbia, 2020 .............. 17
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 9
Table 1. Number of fetal deaths and births and fetal mortality rates for 1990–2020 and early and late fetal deaths and fetal
mortality rates for 2014–2020: United States
Fetal deaths Fetal mortality rate
1
Year Total
2
20–27 weeks
3
28 weeks or more
3
Live births Total
2
20–27 weeks
3
28 weeks or more
3
2020 20,854 10,764 10,090 3,613,647 5.74 2.97 2.78
2019. . . . . . . . . . . . . 21,478 11,216 10,262 3,747,540 5.70 2.98 2.73
2018. . . . . . . . . . . . . 22,459 11,844 10,615 3,791,712 5.89 3.11 2.79
2017. . . . . . . . . . . . . 22,827 11,861 10,966 3,855,500 5.89 3.07 2.84
2016. . . . . . . . . . . . . 23,880 12,486 11,394 3,945,875 6.02 3.15 2.88
2015. . . . . . . . . . . . . 23,776 12,407 11,369 3,978,497 5.94 3.11 2.85
2014
4
. . . . . . . . . . . . 23,980 12,652 11,328 3,988,076 5.98 3.16 2.83
2013. . . . . . . . . . . . . 23,595 --- --- 3,932,181 5.96 --- ---
2012. . . . . . . . . . . . . 24,073 --- --- 3,952,841 6.05 --- ---
2011. . . . . . . . . . . . . 24,289 --- --- 3,953,590 6.11 --- ---
2010. . . . . . . . . . . . . 24,258 --- --- 3,999,386 6.03 --- ---
2009. . . . . . . . . . . . . 24,872 --- --- 4,130,665 5.99 --- ---
2008. . . . . . . . . . . . . 26,335 --- --- 4,247,726 6.16 --- ---
2007. . . . . . . . . . . . . 26,593 --- --- 4,316,233 6.12 --- ---
2006. . . . . . . . . . . . . 25,972 --- --- 4,265,593 6.05 --- ---
2005. . . . . . . . . . . . . 25,894 --- --- 4,138,573 6.22 --- ---
2004. . . . . . . . . . . . . 26,001 --- --- 4,112,055 6.28 --- ---
2003. . . . . . . . . . . . . 26,004 --- --- 4,090,007 6.32 --- ---
2002. . . . . . . . . . . . . 25,943 --- --- 4,021,825 6.41 --- ---
2001. . . . . . . . . . . . . 26,373 --- --- 4,026,036 6.51 --- ---
2000. . . . . . . . . . . . . 27,003 --- --- 4,058,882 6.61 --- ---
1995. . . . . . . . . . . . . 27,294 --- --- 3,899,589 6.95 --- ---
1990. . . . . . . . . . . . . 31,386 --- --- 4,158,445 7.49 --- ---
--- Data not available.
1
Number of fetal deaths in specified group per 1,000 live births and fetal deaths.
2
Fetal deaths with stated or presumed period of gestation of 20 weeks or more.
3
Not stated gestational age proportionally distributed.
4
Beginning with the 2014 data year, the obstetric estimate of gestation at delivery replaced the measure based on the date of last normal menses as the standard for measuring gestational age;
see Technical Notes in this report.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
10 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
Table 2. Fetal deaths and mortality rates, by race and Hispanic origin of mother: United States, 2018–2020
Non-Hispanic, single race
1
Year
All races and
origins
2
White Black
American Indian or
Alaska Native Asian
Native Hawaiian
or Other Pacific
Islander Hispanic
3
Rate
4
2020. . . . . . . . . . . . . 5.74 4.73 10.34 7.84 3.93 10.59 4.86
2019. . . . . . . . . . . . . 5.70 4.71 10.41 7.47 4.02 10.03 4.79
2018. . . . . . . . . . . . . 5.89 4.89 10.64 6.25 4.26 9.93 5.06
Number of deaths
2020. . . . . . . . . . . . . 20,854 8,753 5,536 212 864 103 4,231
2019. . . . . . . . . . . . . 21,478 9,067 5,766 214 963 99 4,264
2018. . . . . . . . . . . . . 22,459 9,621 5,938 183 1,029 95 4,510
1
Race and Hispanic origin are reported separately on reports of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race
categories are consistent with the 1997 Office of Management and Budget standards. Single race is defined as only one race reported on the report of fetal death.
2
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
3
Includes all people of Hispanic origin of any race.
4
Number of fetal deaths in specified group per 1,000 live births and fetal deaths.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 11
Table 3. Fetal deaths and mortality rates, by Hispanic origin of mother: United States, 2018–2020
Year Total Mexican Puerto Rican Cuban Dominican
Central and
South American
Other and
unknown Hispanic
Rate
1
2020. . . . . . . . . . . . . 4.86 4.79 4.98 5.23 4.41 4.49 5.87
2019. . . . . . . . . . . . . 4.79 4.86 5.17 4.71 4.75 4.12 5.29
2018. . . . . . . . . . . . . 5.06 5.19 5.07 4.16 5.09 4.90 4.90
Number of deaths
2020. . . . . . . . . . . . . 4,231 2,312 349 122 140 766 542
2019. . . . . . . . . . . . . 4,264 2,427 369 112 155 683 518
2018. . . . . . . . . . . . . 4,510 2,587 365 98 164 726 570
1
Number of fetal deaths in specified group per 1,000 live births and fetal deaths.
NOTE: In this table, Hispanic women are classified only by place of origin; non-Hispanic women are not shown.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
12 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
Table 4. Total, early, and late fetal deaths and mortality rates, by age and race and Hispanic origin of mother: United States,
2020
Race and Hispanic origin
and age of mother
Fetal deaths Fetal mortality rate
1
Total 20–27 weeks
2
28 weeks or more
2
Total 20–27 weeks
2
28 weeks or more
2
All races
3
. . . . . . . . . . . . . . . . . . . . . . . . . 20,854 10,764 10,090 5.74 2.97 2.78
Under 15 . . . . . . . . . . . . . . . . . . . . . . . 24 18 6 13.42 * *
15–19 . . . . . . . . . . . . . . . . . . . . . . . . . . 1,140 607 533 7.16 3.83 3.36
15–17 . . . . . . . . . . . . . . . . . . . . . . . . 296 178 118 7.61 4.59 3.05
18–19 . . . . . . . . . . . . . . . . . . . . . . . . 844 429 415 7.02 3.58 3.46
20–24 . . . . . . . . . . . . . . . . . . . . . . . . . . 3,905 1,980 1,925 5.83 2.97 2.88
25–29 . . . . . . . . . . . . . . . . . . . . . . . . . . 5,450 2,738 2,712 5.29 2.67 2.64
30–34 . . . . . . . . . . . . . . . . . . . . . . . . . . 5,511 2,831 2,680 5.12 2.64 2.50
35–39 . . . . . . . . . . . . . . . . . . . . . . . . . . 3,677 2,002 1,675 6.48 3.54 2.96
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . 1,033 539 494 8.49 4.45 4.08
45 and over . . . . . . . . . . . . . . . . . . . . . 114 49 65 12.20 5.28 6.99
Non-Hispanic, single race
4
:
White . . . . . . . . . . . . . . . . . . . . . . . . . . 8,753 4,295 4,458 4.73 2.32 2.41
Under 15 . . . . . . . . . . . . . . . . . . . . . . 3 2 1 * * *
15–19 . . . . . . . . . . . . . . . . . . . . . . . . 363 185 178 6.63 3.39 3.26
15–17 . . . . . . . . . . . . . . . . . . . . . . 86 56 30 7.83 5.11 2.75
18–19 . . . . . . . . . . . . . . . . . . . . . . 277 129 148 6.32 2.95 3.39
20–24 . . . . . . . . . . . . . . . . . . . . . . . . 1,419 681 738 4.81 2.31 2.51
25–29 . . . . . . . . . . . . . . . . . . . . . . . . 2,340 1,104 1,236 4.42 2.09 2.34
30–34 . . . . . . . . . . . . . . . . . . . . . . . . 2,612 1,276 1,336 4.30 2.10 2.20
35–39 . . . . . . . . . . . . . . . . . . . . . . . . 1,565 811 754 5.16 2.68 2.49
40–44 . . . . . . . . . . . . . . . . . . . . . . . . 411 215 196 7.17 3.76 3.43
45 and over . . . . . . . . . . . . . . . . . . . . 40 20 20 9.90 4.97 4.97
Black . . . . . . . . . . . . . . . . . . . . . . . . . . . 5,536 3,047 2,489 10.34 5.72 4.68
Under 15 . . . . . . . . . . . . . . . . . . . . . . 12 9 3 * * *
15–19 . . . . . . . . . . . . . . . . . . . . . . . . 381 206 175 11.03 6.00 5.10
15–17 . . . . . . . . . . . . . . . . . . . . . . 108 63 45 11.90 6.97 4.99
18–19 . . . . . . . . . . . . . . . . . . . . . . 273 143 130 10.73 5.65 5.14
20–24 . . . . . . . . . . . . . . . . . . . . . . . . 1,260 685 575 9.99 5.46 4.58
25–29 . . . . . . . . . . . . . . . . . . . . . . . . 1,504 807 697 9.51 5.13 4.43
30–34 . . . . . . . . . . . . . . . . . . . . . . . . 1,255 689 566 9.80 5.40 4.44
35–39 . . . . . . . . . . . . . . . . . . . . . . . . 847 508 339 12.28 7.40 4.95
40–44 . . . . . . . . . . . . . . . . . . . . . . . . 247 133 114 14.18 7.69 6.59
45 and over . . . . . . . . . . . . . . . . . . . . 30 10 20 20.28 * 13.61
Hispanic
5
. . . . . . . . . . . . . . . . . . . . . . . . . 4,231 2,165 2,066 4.86 2.49 2.38
Under 15 . . . . . . . . . . . . . . . . . . . . . . . 6 4 2 * * *
15–19 . . . . . . . . . . . . . . . . . . . . . . . . . . 284 153 131 4.81 2.60 2.22
15–17 . . . . . . . . . . . . . . . . . . . . . . . . 81 45 36 5.04 2.81 2.25
18–19 . . . . . . . . . . . . . . . . . . . . . . . . 203 108 95 4.72 2.52 2.22
20–24 . . . . . . . . . . . . . . . . . . . . . . . . . . 890 432 458 4.45 2.16 2.29
25–29 . . . . . . . . . . . . . . . . . . . . . . . . . . 1,026 512 514 4.08 2.04 2.05
30–34 . . . . . . . . . . . . . . . . . . . . . . . . . . 989 527 462 4.70 2.51 2.20
35–39 . . . . . . . . . . . . . . . . . . . . . . . . . . 751 398 353 6.38 3.39 3.01
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . 255 125 130 8.58 4.22 4.39
45 and over . . . . . . . . . . . . . . . . . . . . . 30 13 17 15.41 * *
* Estimate does not meet National Center for Health Statistics standards of reliability or precision; based on fewer than 20 fetal deaths in the numerator.
1
Rate per 1,000 live births and fetal deaths in specified group.
2
Fetal deaths with gestational age not stated were proportionally distributed; see Technical Notes in this report.
3
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
4
Race and Hispanic origin are reported separately on reports of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race
categories are consistent with the 1997 Office of Management and Budget standards; see Technical Notes in this report. Single race is defined as only one race reported on the report of fetal
death.
5
Includes all people of Hispanic origin of any race.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 13
Table 5. Fetal mortality rates, by tobacco use during pregnancy, age, and race and Hispanic origin of mother:
United States, 2020
Tobacco use during pregnancy and
race and Hispanic origin of mother
Fetal
deaths All ages Under 20 20–24 25–29 30–34 35–39 40–54 Not stated
All races and origins
1
Number Fetal mortality rate
2
Number
Total . . . . . . . . . . . . . . . . . . . . . . . . .
20,854 5.74 7.23 5.83 5.29 5.12 6.48 8.76 1,661
Yes . . . . . . . . . . . . . . . . . . . . . . . 1,753 8.71 7.63 6.73 8.00 9.71 12.30 12.99 …
No . . . . . . . . . . . . . . . . . . . . . . . . . 17,440 5.10 6.62 5.33 4.66 4.52 5.68 7.87 …
Non-Hispanic, single race
3
White:
Total . . . . . . . . . . . . . . . . . . . . . . . 8,753 4.73 6.63 4.81 4.42 4.30 5.16 7.35 610
Yes . . . . . . . . . . . . . . . . . . . . . . 1,153 7.65 6.93 5.77 7.45 8.12 10.95 11.92 …
No . . . . . . . . . . . . . . . . . . . . . . . 6,990 4.12 6.03 4.37 3.80 3.76 4.38 6.50 …
Black:
Total . . . . . . . . . . . . . . . . . . . . . . . 5,536 10.34 11.21 9.99 9.51 9.80 12.28 14.66 405
Yes . . . . . . . . . . . . . . . . . . . . . . 356 14.68 * 13.10 11.97 16.23 20.49 * …
No . . . . . . . . . . . . . . . . . . . . . . . 4,775 9.40 10.34 9.19 8.70 8.71 11.03 13.41 …
Hispanic
4
Total . . . . . . . . . . . . . . . . . . . . . . . . . 4,231 4.86 4.85 4.45 4.08 4.70 6.38 9.00 259
Yes . . . . . . . . . . . . . . . . . . . . . . . . 118 9.50 * 7.89 7.63 12.67 * * …
No . . . . . . . . . . . . . . . . . . . . . . . . . 3,854 4.50 4.53 4.12 3.77 4.32 5.98 8.39 …
… Category not applicable.
* Estimate does not meet National Center for Health Statistics standards of reliability or precision; based on fewer than 20 fetal deaths in the numerator.
1
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
2
Rate per 1,000 live births and fetal deaths in specified group.
3
Race and Hispanic origin are reported separately on the report of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race
categories are consistent with the 1997 Office of Management and Budget standards; see Technical Notes in this report. Single race is defined as only one race reported on the report of fetal
death.
4
Includes all people of Hispanic origin of any race; see Technical Notes in this report.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
14 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
Table 6. Fetal deaths and mortality rates, by birthweight, gestational age, and race and Hispanic origin of mother: United States, 2020
Birthweight (grams) and race
and Hispanic origin of mother Total
Gestational age (weeks)
Fetal
mortality rate
1
20–23 24–27 28–31 32–33 34–36 37–38 39–40 41 42 or more Not stated
All races
2
. . . . . . . . . . . . . . . . . . . . 20,854 7,427 3,266 2,564 1,485 2,636 1,948 1,234 117 39 138 5.74
Less than 500 . . . . . . . . . . . . . . . 6,893 5,535 1,073 174 25 28 19 12 – 1 26 590.00
500–749 . . . . . . . . . . . . . . . . . . . 2,222 905 991 256 43 14 5 2 – 1 5 213.53
750–999 . . . . . . . . . . . . . . . . . . . 1,371 143 624 493 57 34 7 3 – – 10 124.73
1,000–1,249 . . . . . . . . . . . . . . . . 995 49 205 527 129 65 8 5 – – 7 81.02
1,250–1,499 . . . . . . . . . . . . . . . . 915 27 60 445 217 127 28 5 1 1 4 59.57
1,500–1,999 . . . . . . . . . . . . . . . . 1,693 21 35 394 561 526 114 34 2 1 5 28.29
2,000–2,499 . . . . . . . . . . . . . . . . 1,737 – 22 99 301 891 308 99 7 4 6 9.01
2,500–2,999 . . . . . . . . . . . . . . . . 1,488 – 9 24 52 536 569 264 19 5 10 2.15
3,000–3,499 . . . . . . . . . . . . . . . . 1,165 – – 14 21 201 474 410 33 8 4 0.83
3,500–3,999 . . . . . . . . . . . . . . . . 551 – – 2 2 71 197 244 25 7 3 0.58
4,000 or more . . . . . . . . . . . . . . 353 – – – 1 49 146 120 26 8 3 1.30
Not stated . . . . . . . . . . . . . . . . . . 1,471 747 247 136 76 94 73 36 4 3 55 …
Fetal mortality rate
1
. . . . . . . . . . 5.74 540.18 172.67 73.20 34.41 9.77 1.94 0.60 0.66 4.38 … …
Non-Hispanic, single race
3
:
White . . . . . . . . . . . . . . . . . . . . . 8,753 2,968 1,310 1,038 635 1,164 908 621 53 22 34 4.73
Less than 500 . . . . . . . . . . . . . 2,769 2,199 441 78 11 13 15 7 – – 5 645.45
500–749 . . . . . . . . . . . . . . . . . 855 335 397 98 15 7 2 1 – – – 236.58
750–999 . . . . . . . . . . . . . . . . . 560 55 252 205 26 13 3 3 – – 3 137.80
1,000–1,249 . . . . . . . . . . . . . . 388 18 76 206 54 28 2 3 – – 1 80.03
1,250–1,499 . . . . . . . . . . . . . . 355 13 25 177 70 56 12 1 – – 1 56.41
1,500–1,999 . . . . . . . . . . . . . . 705 8 12 171 239 212 43 18 – 1 1 27.55
2,000–2,499 . . . . . . . . . . . . . . 742 – 7 39 147 377 128 37 4 2 1 8.86
2,500–2,999 . . . . . . . . . . . . . . 737 – 7 12 22 280 276 123 9 4 4 2.44
3,000–3,499 . . . . . . . . . . . . . . 582 – – 5 13 86 246 212 13 5 2 0.83
3,500–3,999 . . . . . . . . . . . . . . 301 – – – 1 37 103 143 12 3 2 0.55
4,000 or more . . . . . . . . . . . . . 144 – – – – 23 47 54 13 6 1 0.85
Not stated . . . . . . . . . . . . . . . . 615 340 93 47 37 32 31 19 2 1 13 …
Fetal mortality rate
1
. . . . . . . . . 4.73 596.58 187.60 70.52 32.48 9.08 1.89 0.57 0.52 3.75 … …
Black . . . . . . . . . . . . . . . . . . . . . . 5,536 2,061 963 757 407 652 414 218 11 12 41 10.34
Less than 500 . . . . . . . . . . . . . 1,976 1,593 312 52 7 3 1 1 – – 7 522.47
500–749 . . . . . . . . . . . . . . . . . 661 245 306 86 16 4 1 – – 1 2 182.65
750–999 . . . . . . . . . . . . . . . . . 394 40 194 133 12 11 1 – – – 3 115.17
1,000–1,249 . . . . . . . . . . . . . . 304 10 56 181 36 18 1 – – – 2 83.89
1,250–1,499 . . . . . . . . . . . . . . 252 3 15 130 68 27 5 3 – 1 – 58.78
1,500–1,999 . . . . . . . . . . . . . . 465 10 9 99 161 142 34 7 – – 3 30.49
2,000–2,499 . . . . . . . . . . . . . . 444 – 3 22 74 234 79 28 – 2 2 9.74
2,500–2,999 . . . . . . . . . . . . . . 316 – 1 5 12 117 125 50 2 – 4 2.30
3,000–3,499 . . . . . . . . . . . . . . 215 – – 2 5 45 85 72 4 1 1 1.08
3,500–3,999 . . . . . . . . . . . . . . 92 – – 1 1 14 34 37 1 3 1 0.96
4,000 or more . . . . . . . . . . . . . 67 – – – – 10 34 17 3 2 1 3.02
Not stated . . . . . . . . . . . . . . . . 350 160 67 46 15 27 14 3 1 2 15 …
Fetal mortality rate
1
. . . . . . . . . 10.34 478.19 160.61 82.84 41.70 12.74 2.50 0.82
* *
… …
See footnotes at end of table.
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 15
Table 6. Fetal deaths and mortality rates, by birthweight, gestational age, and race and Hispanic origin of mother: United States, 2020—Con.
Birthweight (grams) and race
and Hispanic origin of mother Total
Gestational age (weeks)
Fetal
mortality rate
1
20–23 24–27 28–31 32–33 34–36 37–38 39–40 41 42 or more Not stated
Hispanic
4
. . . . . . . . . . . . . . . . . . . . 4,231 1,517 635 501 287 551 413 266 33 3 25 4.86
Less than 500 . . . . . . . . . . . . . . . 1,426 1,158 212 31 5 7 1 4 – – 8 588.28
500–749 . . . . . . . . . . . . . . . . . . . 472 200 203 52 9 3 2 1 – – 2 213.86
750–999 . . . . . . . . . . . . . . . . . . . 268 29 115 99 13 8 3 – – – 1 110.61
1,000–1,249 . . . . . . . . . . . . . . . . 193 15 46 84 27 16 3 2 – – – 74.17
1,250–1,499 . . . . . . . . . . . . . . . . 201 4 8 94 55 30 7 1 – – 2 61.88
1,500–1,999 . . . . . . . . . . . . . . . . 336 2 8 84 93 116 25 7 1 – – 26.39
2,000–2,499 . . . . . . . . . . . . . . . . 378 – 10 25 57 185 74 24 2 – 1 9.06
2,500–2,999 . . . . . . . . . . . . . . . . 271 – 1 5 11 91 95 60 6 1 1 1.61
3,000–3,499 . . . . . . . . . . . . . . . . 230 – – 5 3 44 89 76 12 1 – 0.65
3,500–3,999 . . . . . . . . . . . . . . . . 117 – – 1 – 16 45 47 7 1 – 0.52
4,000 or more . . . . . . . . . . . . . . 108 – – – 1 14 50 37 5 – 1 1.82
Not stated . . . . . . . . . . . . . . . . . . 231 109 32 21 13 21 19 7 – – 9 …
Fetal mortality rate
1
. . . . . . . . . . 4.86 513.54 152.75 64.45 30.01 8.61 1.64 0.54 0.86 * … …
– Quantity zero.
… Category not applicable.
* Estimate does not meet National Center for Health Statistics standards of reliability or precision; based on fewer than 20 fetal deaths in the numerator.
1
Rate per 1,000 live births and fetal deaths in specified group.
2
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
3
Race and Hispanic origin are reported separately on the report of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race categories are consistent with the 1997 Office of Management
and Budget standards; see Technical Notes in this report. Single race is defined as only one race reported on the report of fetal death.
4
Includes all people of Hispanic origin of any race; see Technical Notes in this report.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
16 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
Area Fetal deaths
1
Fetal mortality rate
2
Total . . . . . . . . . . . . . . . . . . 20,854 5.74
Alabama . . . . . . . . . . . . . 489 8.41
Alaska . . . . . . . . . . . . . . . 54 5.67
Arizona . . . . . . . . . . . . . . 459 5.93
Arkansas . . . . . . . . . . . . . 318 8.94
California . . . . . . . . . . . . 2,196 5.20
Colorado . . . . . . . . . . . . . 327 5.29
Connecticut . . . . . . . . . . 149 4.43
Delaware . . . . . . . . . . . . . 57 5.46
District of Columbia . . . . 70 7.83
Florida . . . . . . . . . . . . . . 1,458 6.91
Georgia . . . . . . . . . . . . . . 1,007 8.16
Hawaii . . . . . . . . . . . . . . . 103 6.48
Idaho . . . . . . . . . . . . . . . 117 5.40
Illinois . . . . . . . . . . . . . . . 754 5.62
Indiana . . . . . . . . . . . . . . 476 6.02
Iowa . . . . . . . . . . . . . . . . 166 4.58
Kansas . . . . . . . . . . . . . . 168 4.86
Kentucky . . . . . . . . . . . . . 327 6.29
Louisiana . . . . . . . . . . . . 322 5.59
Maine . . . . . . . . . . . . . . . 74 6.37
Maryland . . . . . . . . . . . . 466 6.75
Massachusetts . . . . . . . . 278 4.17
Michigan . . . . . . . . . . . . . 612 5.85
Minnesota . . . . . . . . . . . . 343 5.38
Mississippi . . . . . . . . . . . 380 10.60
Missouri . . . . . . . . . . . . . 431 6.18
Montana . . . . . . . . . . . . . 44 4.06
Nebraska . . . . . . . . . . . . 104 4.26
Nevada . . . . . . . . . . . . . . 260 7.67
New Hampshire . . . . . . . 54 4.56
New Jersey . . . . . . . . . . . 658 6.67
New Mexico . . . . . . . . . . 77 3.50
New York . . . . . . . . . . . . 1,338 6.35
North Carolina . . . . . . . . 680 5.79
North Dakota . . . . . . . . . 61 6.03
Ohio . . . . . . . . . . . . . . . . 746 5.74
Oklahoma . . . . . . . . . . . . 302 6.30
Oregon . . . . . . . . . . . . . . 205 5.12
Pennsylvania . . . . . . . . . 668 5.09
Rhode Island . . . . . . . . . 63 6.20
Area Fetal deaths
1
Fetal mortality rate
2
South Carolina . . . . . . . . 310 5.53
South Dakota
3
. . . . . . . . 67 6.08
Tennessee . . . . . . . . . . . . 520 6.56
Texas . . . . . . . . . . . . . . . 1,492 4.04
Utah . . . . . . . . . . . . . . . . 235 5.12
Vermont . . . . . . . . . . . . . 27 5.23
Virginia . . . . . . . . . . . . . . 466 4.89
Washington . . . . . . . . . . 448 5.36
West Virginia . . . . . . . . . 80 4.60
Wisconsin . . . . . . . . . . . . 317 5.20
Wyoming . . . . . . . . . . . . 31 5.03
American Samoa . . . . . . --- ---
Guam . . . . . . . . . . . . . . . 49 16.42
Northern Marianas . . . . . --- ---
Puerto Rico . . . . . . . . . . 217 11.33
Virgin Islands . . . . . . . . . --- ---
--- Data not available.
1
Fetal deaths with stated or presumed period of gestation of 20 weeks or more.
2
Number of fetal deaths per 1,000 live births and fetal deaths.
3
State reports only fetal deaths of 500 grams or more.
NOTES: American Samoa did not report data for 2020. Data for the Northern Marianas and
the Virgin Islands were excluded due to small numbers.
SOURCE: National Center for Health Statistics, National Vital Statistics System.
Table 7. Fetal deaths at 20 weeks of gestation or more and fetal mortality rates: United States and each state and territory, 2020
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 17
Table 8. Fetal deaths and percentage of total deaths for the five selected causes, by race and Hispanic origin of mother: 43 states
and the District of Columbia, 2020
Rank Cause and race and Hispanic origin of mother Deaths Percent
All races and origins
1
… All causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15,740 100.0
1 Fetal death of unspecified cause (P95) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,979 31.6
2 Fetus affected by complications of placenta, cord and membranes (P02) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3,848 24.4
3 Fetus affected by maternal complications of pregnancy (P01) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,899 12.1
4 Fetus affected by maternal conditions that may be unrelated to present pregnancy (P00) . . . . . . . . . . . . . . . . . . . . . . . . . . 1,712 10.9
5 Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,661 10.6
… All other causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,641 10.4
Non-Hispanic, single-race White
2
… All causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7,207 100.0
1 Fetal death of unspecified cause (P95) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,332 32.4
2 Fetus affected by complications of placenta, cord and membranes (P02) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,790 24.8
3 Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 905 12.6
4 Fetus affected by maternal complications of pregnancy (P01) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 720 10.0
5 Fetus affected by maternal conditions that may be unrelated to present pregnancy (P00) . . . . . . . . . . . . . . . . . . . . . . . . . . 708 9.8
… All other causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 752 10.4
Non-Hispanic, single-race Black
2
… All causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4,146 100.0
1 Fetal death of unspecified cause (P95) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,253 30.2
2 Fetus affected by complications of placenta, cord and membranes (P02) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,052 25.4
3 Fetus affected by maternal complications of pregnancy (P01) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 605 14.6
4 Fetus affected by maternal conditions that may be unrelated to present pregnancy (P00) . . . . . . . . . . . . . . . . . . . . . . . . . . 571 13.8
5 Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 261 6.3
… All other causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 404 9.7
Hispanic
3
… All causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,810 100.0
1 Fetal death of unspecified cause (P95) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 858 30.5
2 Fetus affected by complications of placenta, cord and membranes (P02) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 652 23.2
3 Fetus affected by maternal complications of pregnancy (P01) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 381 13.6
4 Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 329 11.7
5 Fetus affected by maternal conditions that may be unrelated to present pregnancy (P00) . . . . . . . . . . . . . . . . . . . . . . . . . . 277 9.9
… All other causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 313 11.1
… Category not applicable.
1
Includes fetal deaths to race and Hispanic-origin groups not shown separately.
2
Race and Hispanic origin are reported separately on the report of fetal death; people of Hispanic origin may be of any race. In this table, non-Hispanic women are classified by race. Race
categories are consistent with the 1997 Office of Management and Budget standards; see Technical Notes in this report. Single race is defined as only one race reported on the report of fetal
death.
3
Includes all people of Hispanic origin of any race; see Technical Notes in this report.
NOTES: Findings exclude data for jurisdictions (Georgia, Hawaii, Michigan, Mississippi, New York City, North Dakota, and Vermont) for which the cause of death was unspecified (P95) for
50% of records or more. Findings also exclude data for California, which did not report cause of death based on the 2003 revision of the U.S. Standard Report of Fetal Death.
SOURCE: National Center for Health Statistics, National Vital Statistics System.

18 National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
published in this report by variables with a substantial percentage
of unknown responses (such as birthweight) may understate the
true rates of fetal mortality for that characteristic.
2003 revision of U.S. Standard Report of Fetal
Death
Data for 2018–2020 presented in this report are based on
the 2003 revision of the U.S. Standard Report of Fetal Death;
data for earlier years are based on both the 1989 and the 2003
fetal death report revisions. The 2003 revision is described in
detail elsewhere (16).
Computation of rates
Fetal mortality rates in this report are computed as the
number of fetal deaths at 20 weeks of gestation or more per
1,000 live births and fetal deaths at 20 weeks or more. The
denominators for all fetal mortality rates are live births plus fetal
deaths in the specified gestational age group, thus representing
the population at risk of the event.
In each case, the fetal deaths included in the denominator of
each rate mirror the fetal deaths included in the numerator. A
previous NCHS report (17) contains information on the historical
development of various perinatal measures. An asterisk (*) is
shown in place of any rate based on fewer than 20 fetal deaths
in the numerator.
Hispanic origin and race
Hispanic origin
Hispanic origin and race are reported separately on the report
of fetal death. Data are presented in some tables for specific
Hispanic subgroups: Mexican, Puerto Rican, Cuban, Central and
South American, Dominican, and Other and unknown Hispanic.
Data are presented separately for Dominican women beginning
in 2018. Data for this subgroup had previously been included
in the category Other and unknown Hispanic. In tabulations of
fetal death data by race and Hispanic origin, data for people of
Hispanic origin are not further classified by race because the
vast majority of fetal deaths to Hispanic women are reported as
White.
Race
This report presents data on race and Hispanic origin based
on the 1997 Office of Management and Budget (OMB) standards
(10). The 2003 revision of the U.S. Standard Report of Fetal
Death requires the reporting of a minimum of five race categories
and allows for the reporting of race either alone (single race) or
in combination (more than one race or multiple races) for the
mother (9), in accordance with OMB’s 1997 revised standards
Fetal mortality rate =
Fetal deaths at 20 weeks
of gestatio
nn or more
Live births and fetal deaths at
20 weeks or more
•• 1,000
Technical Notes
Definition of fetal death
Fetal death means death prior to the complete expulsion or
extraction from its mother of a product of human conception,
irrespective of the duration of pregnancy and which is not an
induced termination of pregnancy. The death is indicated by the
fact that after such expulsion or extraction, the fetus does not
breathe or show any other evidence of life such as beating of
the heart, pulsation of the umbilical cord, or definite movement
of voluntary muscles. Heartbeats are to be distinguished
from transient cardiac contractions; respirations are to be
distinguished from fleeting respiratory efforts or gasps.
This definition (14) has been adopted by the Centers for
Disease Control and Prevention, National Center for Health
Statistics (NCHS) as the nationally recommended standard
and is based on the definition published by the World Health
Organization in 1950 and revised in 1988. The term fetal death
is defined on an all-inclusive basis to end confusion arising
from the use of such terms as stillbirth, spontaneous abortion,
and miscarriage. All U.S. states and registration areas have
definitions similar to the standard definition, except for Puerto
Rico and Wisconsin, which have no formal definition (15). Fetal
deaths do not include induced terminations of pregnancy.
Reporting requirements for fetal death data
There is variation among states in reporting requirements
(2) and possibly in completeness of reporting for fetal death
data, which can have important implications for comparisons
of fetal mortality rates by state. The majority of states require
reporting of fetal deaths at 20 weeks of gestation or more, or
a minimum birthweight of 350 grams (roughly equal to 20
weeks), or some combination of the two. However, six states,
New York City, American Samoa, and the U.S. Virgin Islands
require reporting of fetal deaths at all periods of gestation, two
states require reporting beginning at 12 weeks of gestation, and
one state requires reporting beginning at 16 weeks of gestation.
At the other end of the spectrum, one state (South Dakota)
requires reporting of fetal deaths with birthweights of 500 grams
or more (roughly equal to 22 weeks of gestation). Areas that
report fetal deaths at all periods of gestation appear to have a
higher percentage of fetal deaths occurring at 20–27 weeks of
gestation than those that begin reporting at later gestational ages.
Table B presents fetal mortality rates for fetal deaths at 24 weeks
of gestation or more for a combined 3-year period to better
account for state differences in reporting requirements and
improve on the reliability of rates based on smaller numbers.
Aside from this exception, this report presents data on fetal
deaths with a stated or presumed period of gestation of 20 weeks
or more.
Percentage of unknown responses
In the tables in this report, unknown responses are shown
in frequencies tables but are excluded from the computation of
percent distributions and fetal mortality rates. As a result, rates
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022 19
(10). The five categories for race specified in the revised
standards are: American Indian or Alaska Native, Asian, Black
or African American, Native Hawaiian or Other Pacific Islander,
and White.
Beginning in 2018, all states and the District of Columbia,
in addition to Guam, the Northern Marianas, Puerto Rico, and
the Virgin Islands were reporting race on fetal death reports
according to the 1997 revised OMB standards. In 2020,
2.0% of women in the United States reported more than one
race. Before this time, the number of states that reported
multiple-race information varied widely, increasing from 1 state
in 2003 to all 50 states, the District of Columbia, Guam, the
Northern Marianas, Puerto Rico, and the Virgin Islands in 2018.
Period of gestation
Beginning with the 2014 data year, NCHS began using the
obstetric estimate of gestation at delivery (OE) as the primary
measure for estimating gestational age (18). The OE data are
edited for gestational ages that are clearly inconsistent with
birthweight. If the OE is not reported or is inconsistent with
birthweight, the last menstrual period (LMP)-based gestational
age is used (0.6% of fetal death records and 0.1% of live birth
records in 2020). These procedures are described in more detail
elsewhere (19).
See the “User Guide to the 2017 Fetal Death Data File” for
a more detailed description of the transition and Table 1 of the
“User Guide to the 2018 Fetal Death Data File” for trends in
total, early, and late fetal mortality based on both the OE- and
LMP-based measures (20,21).
Gestational age not stated
Fetal deaths with not-stated gestational age are presumed to
be 20 weeks of gestation or more if the state requires reporting
of all fetal deaths at 20 weeks or more, or if the fetus weighed
350 grams or more in those states requiring reporting of all fetal
deaths regardless of gestational age. In Tables 1 and 4, fetal
deaths with not-stated gestational age are allocated to the
20–27 week and 28 weeks or more categories according to
the proportion of fetal deaths with stated gestational age that
fall into each category (proportional distribution). Similarly, for
Table B, fetal deaths with not-stated gestational age are
proportionally distributed into the 20–23 week and 24 weeks or
more categories. Proportional distribution is not performed for
data in tables that show more detailed gestational age categories
(Table 6). The allocation of not-stated gestational age for fetal
deaths is made individually for each maternal age, race and
Hispanic-origin group, and state in the computation of fetal
mortality rates.
Cause of death
Cause-of-death data are included for the 43 states and the
District of Columbia that reported cause of death based on the
2003 revision of the U.S. Standard Report of Fetal Death and met
the reporting requirement of having less than 50% of records
assigned to unspecified cause (P95) (cause-of-death data did not
meet these requirements for California, Georgia, Hawaii, Michigan,
Mississippi, New York City, North Dakota, and Vermont).
Random variation in fetal mortality
Please see the “User Guide to the 2020 Fetal Death Public
Use File” (2) for more detailed information and formulas.
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551, MS P08
Hyattsville, MD 20782–2064
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551, MS P08
Hyattsville, MD 20782–2064
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551, MS P08
Hyattsville, MD 20782–2064
FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551, MS P08
Hyattsville, MD 20782–2064
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
National Vital Statistics Reports, Vol. 71, No. 4, August 4, 2022
For more NCHS NVSRs, visit:
https://www.cdc.gov/nchs/products/nvsr.htm.
For e-mail updates on NCHS publication releases, subscribe online at: https://www.cdc.gov/nchs/email-updates.htm.
For questions or general information about NCHS: Tel: 1–800–CDC–INFO (1–800–232–4636) • TTY: 1–888–232–6348
Internet: https://www.cdc.gov/nchs • Online request form: https://www.cdc.gov/info • CS332068
Suggested citation
Gregory ECW, Valenzuela CP, Hoyert DL. Fetal
mortality: United States, 2020. National Vital
Statistics Reports; vol 71 no 4. Hyattsville, MD:
National Center for Health Statistics. 2022.
DOI: https://dx.doi.org/10.15620/cdc:118420.
Copyright information
All material appearing in this report is in
the public domain and may be reproduced
or copied without permission; citation as to
source, however, is appreciated.
National Center for Health Statistics
Brian C. Moyer, Ph.D., Director
Amy M. Branum, Ph.D., Associate
Director for Science
Division of Vital Statistics
Steven Schwartz, Ph.D., Director
Andrés A. Berruti, Ph.D., M.A., Associate
Director for Science
Contents
Abstract .......................................................1
Introduction ....................................................2
Methods .......................................................2
Data sources ..................................................2
Fetal mortality .................................................2
Data limitations ...............................................2
2003 revision of U.S. Standard Report of Fetal Death ..................2
Race and Hispanic origin ........................................3
Fetal deaths by state ............................................3
Cause of death ................................................3
Statistical significance ..........................................3
Results ........................................................3
Trends in fetal mortality .........................................3
Race and Hispanic origin ........................................3
Maternal age ..................................................4
Tobacco use during pregnancy ....................................4
Plurality .....................................................5
Sex of fetus ..................................................6
Period of gestation .............................................6
Birthweight ...................................................6
Fetal mortality rates by state ......................................6
Selected causes of fetal death ....................................7
References .....................................................7
List of Detailed Tables ............................................8
Technical Notes ................................................18
Acknowledgments
This report was prepared in the Division of Vital Statistics (DVS) under the
general direction of Steven Schwartz, Director, DVS; Isabelle Horon, Branch
Chief, Reproductive Statistics Branch (RSB); and Joyce A. Martin, Team Lead,
RSB Birth Team.
